






The upcoming Inflation Reduction Act (IRA) and Maximum Fair Price (MFP) provisions represent one of the most significant shifts in how covered entities manage pharmacy operations, reimbursement, and compliance.
Beginning January 1, selected drugs under Medicare will be reimbursed as normal, but will be at a significantly lower rate, the main change comes from the additional rebate they will receive through the manufacturer.
For covered entities that own and operate retail pharmacies, these changes will directly impact how you manage cash flow, data submission, and audit documentation under your 340B program.
This guide breaks down what’s changing, how it affects your internal pharmacy operations, and the steps your organization can take now to stay prepared.
How the IRA Changes Reimbursement—and Where Beacon and MTF Fit In
The Inflation Reduction Act (IRA) introduces a new layer of coordination between two systems: Beacon, which validates 340B claims and rebate eligibility, and the Manufacturer Transfer Facilitator (MTF), which manages the new Medicare Fair Price (MFP) rebate process.
Beacon remains the clearinghouse for 340B claims, and MTF now oversees MFP rebates under Medicare Part D. Together, they ensure that only one rebate is paid per claim—either a 340B rebate or an MFP rebate, not both.
Here’s how reimbursement now flows under three different scenarios:
The covered entity purchases the drug at full price (WAC) and submits the claim to Beacon.
Beacon verifies eligibility and processes the 340B rebate from the manufacturer back to the covered entity.
In this case, the 340B rebate equals the difference between the full price (WAC) and the 340B ceiling price.
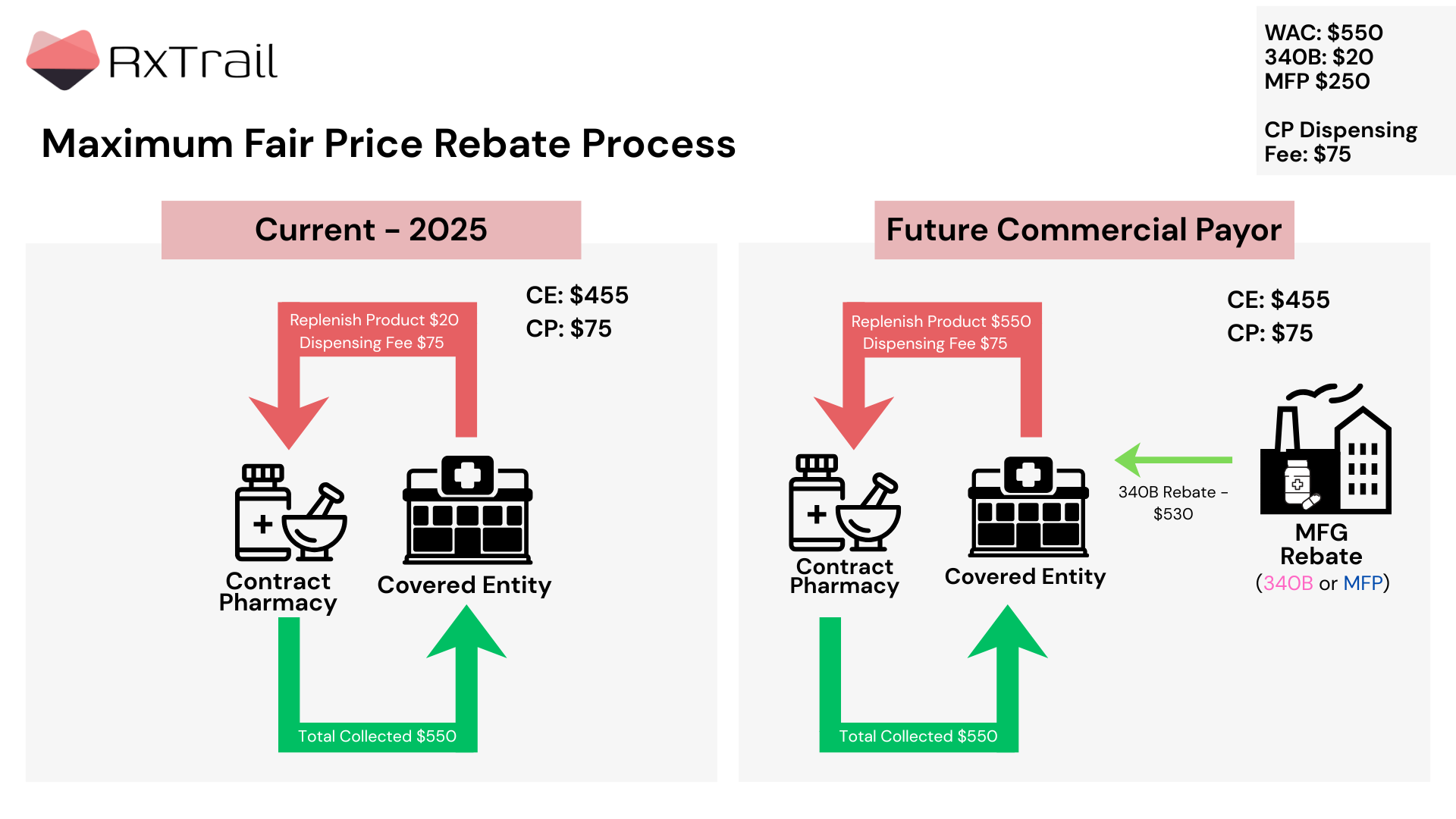
The pharmacy purchases the drug at full price and is reimbursed by Medicare at the Maximum Fair Price (MFP).
The payer submits the claim to the MTF, which then works with Beacon and the manufacturer to confirm rebate eligibility.
If no 340B rebate was paid on that claim, the MFP rebate is issued to the dispensing pharmacy.
Here, the MFP rebate equals WAC minus the negotiated Max Fair Price.
The covered entity again purchases the drug at full price and submits the claim to Beacon.
Beacon verifies 340B eligibility and processes the 340B rebate from the manufacturer.
At the same time, the pharmacy receives reimbursement from Medicare at the Max Fair Price, and the payer submits to the MTF for MFP validation.
Beacon and MTF coordinate to ensure there’s no duplicate discount—if the manufacturer has already paid a 340B rebate, they are not required to pay an additional MFP rebate.

Owning your own retail pharmacy has long provided advantages in control and savings—but the IRA changes that equation.
The biggest impacts you’ll likely face include:
These are not theoretical concerns—they directly affect pharmacy margins, reporting accuracy, and patient reinvestment funds.
Preparation starts with proactive coordination across pharmacy, finance, and compliance teams.
Below are key readiness steps RxTrail recommends for all covered entities with an owned pharmacy:
Validate MTF Enrollment
Confirm your pharmacy is registered with the Medicare Transaction Facilitator (MTF) and your data exchange processes are tested.
Coordinate Beacon Integration
Work with your internal pharmacy and IT teams (or TPA) to confirm how IRA drug claims will be validated through Beacon and reported under 340B.
Model Financial Scenarios
Work with your finance team to estimate rebate lag time and potential impact on cash flow and replenishment cycles.
Audit Workflows for Accuracy
Ensure your dispensing data, claim identifiers, and audit logs can clearly distinguish 340B vs. IRA-covered scripts.
Educate Pharmacy Staff
Provide short briefings for your pharmacy and compliance teams so they understand how these changes will alter normal dispensing and reimbursement routines.
January 1st: Starting January 1, 2026, Medicare will implement its first-ever negotiated prices for 10 high-cost Part D drugs.
At RxTrail, we work with covered entities across the country to help them prepare, adapt, and optimize as new payment and compliance rules take effect.
Our team provides:
Whether you operate one retail pharmacy or a full network, we act as an extension of your team—helping your systems and staff stay aligned as this new model rolls out.
January 1 isn’t just another policy update, it’s a structural change in how covered entity pharmacies function.
By preparing your pharmacy workflows, financial systems, and reporting processes now, you’ll protect your margins, maintain compliance, and ensure patient savings continue to flow where they’re needed most.